DAISY
DAISY is a proof-of-concept decision-support system for A&E patient triage. Patient and clinician trust in the system is essential to its successful introduction into a busy A&E environment. To give transparency of the decisions made by DAISY and to ensure these decisions are in line with those made by a human clinician, we opted for a rules-based decision architecture for patient assessment.
This opens the door to a hybrid-AI solution, where these easily examinable and verifiable rules-based systems can be augmented with traditional techniques, to aid in the healthcare decision-making process.
The triage process
The DAISY system has two primary users: patients and clinicians, each accessing the system in a distinct way as part of a A&E triage process that differs from the typical patient-clinician interaction.
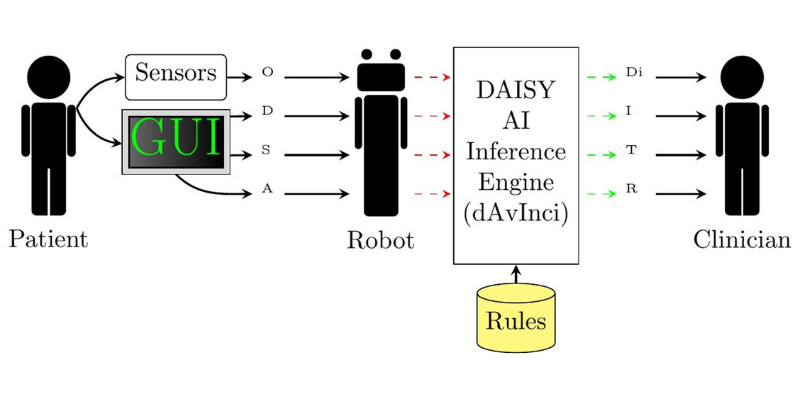
A patient who consents to use DAISY attends a DAISY triage bay containing medical devices (sensors) for collecting objective vital signs (blood pressure, temperature, respiratory rate, pulse rate and blood oxygen saturation). The DAISY software guides the patient through a process that involves the collection of four categories of medically relevant information:
- Objective information (O) is collected by asking the patient to measure their vital signs by using the available medical devices, and input the results of these measurements into the DAISY graphical user interface (GUI).
- Demographic information (D) is obtained by asking the patient for data such as age and gender at birth.
- Subjective information (S) represents the reported patient symptoms and is collected through a series of questions answered by the patient.
- Anatomical information (A) is collected concurrently with subjective data in the symptom reporting section.
The four categories of data are used as input for a decision-support algorithm (dAvInci) that uses a sophisticated set of clinician-specified rules to provide the clinician with potential assessments (Di), alongside suggested investigations (I), low level treatments (T) and referrals (R).
Following the collection of all pertinent information, DAISY returns the patient to the waiting room, where they wait to be collected by clinical staff for healthcare provision or additional investigations.
The clinician receives the output of the dAvInci algorithm within the DAISY system, comprised of a standardised form containing the reported symptoms per anatomical area, relevant demographic information and objective signs reported to the system. It will also include a series of potential assessment outcomes as well as suggested investigations and low-level treatment interventions like painkillers and antibiotics.
The clinician observes this information, making their own assessments in conjunction with the assessments and investigations from DAISY, confirming, adding, or removing where the clinician deems it appropriate.
The ongoing plan decided by the treating clinician is then enacted by clinical staff to confirm potential diagnoses, or the treating clinician attends the patient directly to confirm and refer the patient to an appropriate healthcare setting.
Social, legal, cultural and ethical concerns
One narrow focus of the qualitative-exploratory research project was to explore user requirements that have a social, legal, cultural, and ethical dimension. This included the idea of empathy, and empathetic triage practice, as one overarching component informing these dimensions.
Participants in the study were introduced to the functionality of the DAISY system and questioned about areas of DAISY’s potential utility and benefit, as well as important influences on user's trust, and the role of intuition and non-verbal cues in the patient-clinician relationship and interaction.
All clinicians, regardless of job role, stated the importance of non-verbal cues and intuition when treating patients and the role of local and cultural knowledge. While DAISY was favourably perceived and considered of benefit to the triage process, the need to put safeguards and protections in place was identified.
"I would need to know that DAISY has been properly tested and does not miss anything" (research participant)
Trust, safety and reliability in the diagnostic output were identified as critical factors influencing the utility and wide-spread adoption of DAISY, particularly in the early stages of implementation. The ability to accommodate cultural and social sensitivities, to treat patients with dignity, and to act empathetically were also highlighted.
Proof of concept/solution
The context of the DAISY triage system has two primary methods for interfacing with the system. The primary method is a loop, beginning with the patient who presents with some healthcare concern, then by interacting with the robot, is able to complete a survey to collect medically relevant information, and is supplied to dAvInci where it is processed. The outcome of the dAvInci process is compiled into a standardised form, and sent to a printer, for use by a healthcare expert who can then provide healthcare to the patient.
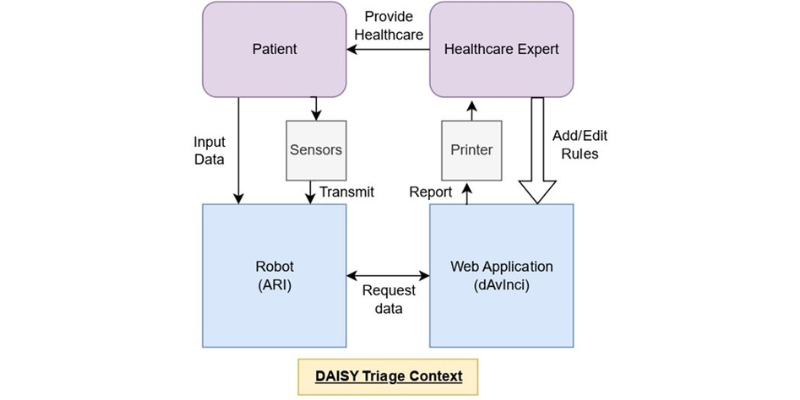
The diagram above shows the context of the DAISY system with the two use cases. The primary use case has arrows in black and the secondary use case shows with a large white arrow. The secondary use case requires minimal interaction with other elements of the DAISY context, as it consists solely of the healthcare expert interacting with the database of rules for the DAISY system and either adding or editing the rules base.
